An MRI fusion biopsy is a combination of an MRI scan and a biopsy.
A common reason for a visit to a urologist is for routine or preventative screenings for cancer. Other times, a regular exam results in the detection of a suspicious growth that requires further evaluation.
This is often the case with prostate cancer, which can be difficult to detect. An MRI fusion biopsy meant to minimize unnecessary procedures and the need for repeat biopsies, as well as provide critical diagnostic information.
When it’s Used
It’s usually after repeated prostate specific antigen (PSA) blood tests show elevated levels that a biopsy is recommended by a urologist. This type of biopsy may also be ordered if something abnormal is detected during a digital rectal examination (DRE). Additionally, a biopsy can avoid confusion with benign prostatic hyperplasia or nodular enlargement – conditions sometimes mistaken for signs of cancer.
Overcoming Shortcomings of a Traditional Biopsy
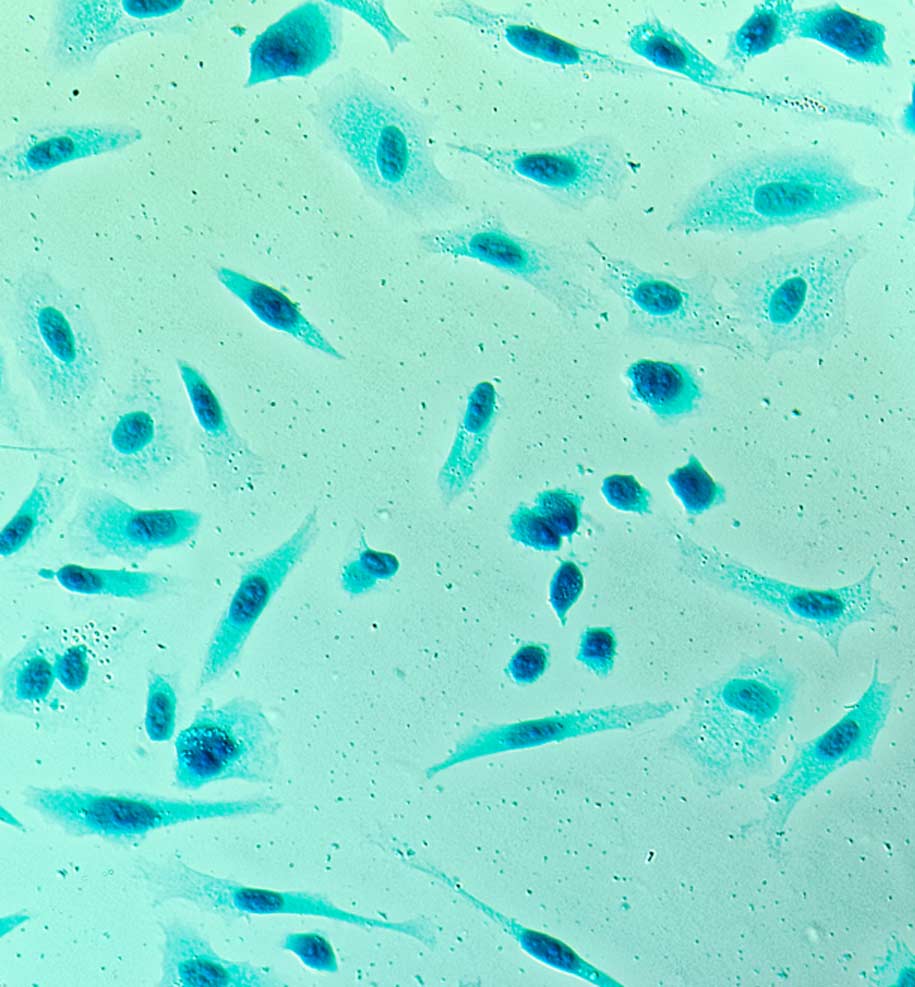
With a traditional biopsy, ultrasound is usually used to help with the accuracy of needle placement. However, the resulting images are sometimes not clear enough to distinguish cancerous tissue from normal tissue, which can make it difficult to zero in on the right tissue to collect for the biopsy. These so-called “random biopsies” sometimes miss harmful tumors or identify ones that are treated unnecessarily. An MRI scan alone can’t be used to diagnose cancer, but the images produced make it easier to identify suspicious areas with better accuracy.
Performing an MRI Fusion Biopsy
The procedure is called an MRI fusion biopsy because it “fuses” together results from an MRI scan and an ultrasound-guided biopsy. The first step in the process is to perform an MRI scan. A device called an endorectal coil is inserted into the rectum to produce internal images. A special contrast dye is administered by IV towards the end of the exam. The images will then be reviewed and any suspicious lesions will be marked. If no “targets” are identified with the MRI, the biopsy part of the procedure may not be necessary.
However, if suspicious areas are identified, the second step in the process is the biopsy itself. A urologist will used the marked images from the MRI. These images are “fused” with real-time images of the area being targeted for testing to improve the accuracy of needle placement for the collection of tissue samples. A standard non-targeted 12-core transrectal ultrasound (TRUS) biopsy may also be performed along with the targeted biopsy. Prior to the biopsy, patients are usually advised to drink a few glasses water since a full bladder makes it easier to view the prostate.
After the Procedure
If no sedation was used, patients will be able to leave immediately after the procedure is completed. There may be a brief period of observation if a light general anesthetic or sedation was requested or recommended. There may be some mild discomfort or slight bleeding in rectal area after the procedure. Overall, however, patient risks are generally considered minimal.
Following an MRI fusion biopsy, it’s often advised that patients continue to take antibiotics for a brief time to reduce infection risk. Results are usually available a day or two after the procedure. The ordering physician will share the results with the patient and make appropriate recommendations based on what was discovered.


